Low-cost, readily deployable respirators could help frontline healthcare workers
As frontline healthcare workers struggle with the national shortage of masks and gear to protect themselves against the coronavirus, Berkeley engineers are working with doctors at UCSF to develop cost-effective powered air-purified respirators (PAPR) that will offer greater protection during higher risk procedures.
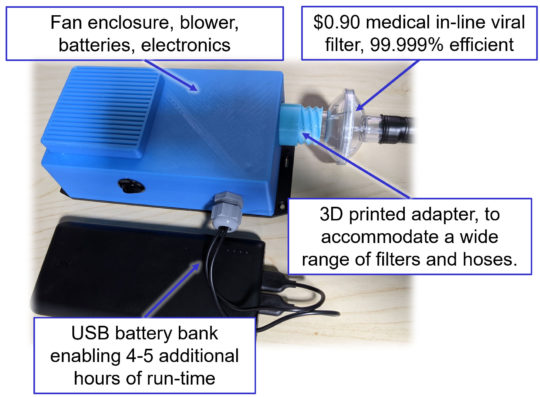
Shown are components of the powered air-purifying respirator prototype developed by UC Berkeley engineers. (Robert Pilawa-Podgurski photo)
Prabal Dutta and Robert Pilawa-Podgurski, UC Berkeley associate professors of electrical engineering and computer sciences, embarked on the project in March after meetings with UCSF anesthesiologists David Robinowitz and Jeffrey Sall. The doctors described major shortages nationwide in personal protective equipment like gloves, gowns and N95 masks.
PAPR devices, which can cost up to $2,000 per unit, were near the bottom of the wish list because the doctors assumed that they would be hard to get and difficult to replicate, Pilawa-Podgurski said.
But the Berkeley engineers, acting on an approach originally proposed to them by Oakland resident Lakin Moser, decided to explore a do-it-yourself PAPR concept. They prioritized a PAPR design that would be medically acceptable, inexpensive to build and rapidly scalable for regional, national and global needs.
The team estimates that their device, made from a combination of standard electronic components and custom electronic circuits and mechanical parts, will cost $200 per unit and be manufactured at scale in weeks.
A PAPR consists of an electronically controlled, battery-powered blower that pulls or pushes air through a filter to remove particles, vapors and gases.
PAPR devices, which are more protective than N95 masks, are used by medical professionals during intubations, nebulizer treatments and high-flow oxygen treatments where the risk of aerosolization of viruses is high. While hospitals may have PAPR units on hand, the need for the devices has exploded due to the surging number of COVID-19 patients.
Unlike N95 masks, filters in PAPR units are designed to be safely reused multiple times because they do not come in direct contact with the user or the user’s breath. PAPR units are also considered more comfortable for prolonged use and can offer a better fit for people who have difficulty getting N95 masks to fit properly.

Dr. Jeffrey Sall, UCSF anesthesiologist, tries on the prototype powered air-purifying respirator developed at UC Berkeley.
The Berkeley engineers, in consultation with the UCSF doctors, ultimately produced a scalable design with off-the-shelf parts sourced from Bay Area manufacturers and major electronics distributors. The prototype includes an easy-to-sanitize enclosure containing rechargeable batteries; power electronics for blower motor control; a $0.90 commercial medical viral filter; an external USB battery pack to provide 4 to 5 extra hours of untethered operation; and a 3D-printed adapter that can accommodate a wide range of hoses and filters. To protect the face, the device is compatible with commercial PAPR hoods, but disposable polyethylene bags, which are widely available at low cost, could also be adapted for use as a hood.
“A key aspect of the design was to source components that are widely available, and to provide modularity to enable swap-in of alternatives if supply chain issues arise,” said Pilawa-Podgurski.
The researchers are continuing to refine the electrical and mechanical design parameters, then placing rapid prototyping orders for the printed circuit board (PCB). Because of the shelter-in-place order, the engineers are assembling the prototype in their garages and basements.
The latest prototype is currently undergoing usability testing at UCSF Medical Center to ensure that the device meets clinical standards.
The team plans to post their design on the web as soon as it is finalized for production so that other people can freely adapt the device for local needs.
“Our hope is that this technology can also be quickly adopted in developing countries, where commercial PAPRs are oftentimes not available due to cost reasons,” explains Pilawa-Podgurski.
Pilawa-Podgurski and his graduate students, Derek Chou and Nathan Pallo, worked on hardware prototyping of the custom blower electronics and lithium-ion battery management, as well as the integration of mechanical components.
Mechanical updates were rapidly iterated thanks to the use of 3D-printing technology and the help of Chris Palmer, manager of the Digital Fabrication Lab at UC Berkeley. Meanwhile, Dutta worked on the system architecture, display electronics, collaboration tools and project documentation. Additionally, high-precision prototyping fixtures were 3D-printed at the Jacobs Institute for Design and Innovation.

Rendering of the blower unit developed for a new, low-cost power air-purified respirator. The components include a nozzle, blower fan, power electronics, air intake opening and optional intake filter. (Nate Pallo image)
The team credits online collaboration tools, digitally exchanged mechanical design files, inexpensive 3D printers at home and high-precision printers on the Berkeley campus, same-day rush PCB manufacturing, overnight electronic component deliveries, and rapid iterations and feedback from UCSF colleagues for the breakneck speed in going from concept to prototype.
Thanks to a seed grant from UCSF, the team is contacting manufacturers to identify a partner that can produce the designs. The team is also seeking additional funds to scale manufacturing to meet expected demands, as well as working to obtain regulatory approval for clinical use.
While the researchers note that this is not yet a certified device, it has been designed to match the safety and performance specifications of commercial PAPR units.
“This was an opportunity to see rapid innovation happen when you get the right people and right technology together, whether at Berkeley, UCSF or unaffiliated volunteers,” Dutta said.
Most importantly, the researchers said they valued the opportunity to move beyond the lab and classroom to help solve an urgent, real-world problem.
“How many opportunities do we get in life to turn toward a big problem and confront it head on?” said Pilawa-Podgurski.