Close-up image of a mechano-node pore sensing (NPS) device.
Close-up image of a mechano-node pore sensing (NPS) device.The power of simplicity
When asked to describe her microfluidic device, Berkeley mechanical engineering professor Lydia Sohn keeps it simple.
“Here’s what I tell my family: It’s like we’re taking a straw, and we’re drinking tapioca boba balls,” says Sohn, who holds the Almy C. Maynard and Agnes Offield Maynard Chair in Mechanical Engineering. “Some boba are bigger than others, and some of these may take more time to squeeze through a straw than smaller ones.”
Now imagine that the boba are cells and the straw is one of many microscopic, fluid-filled channels that the cells must pass through. Along the way, researchers measure different physical characteristics of the cells. That’s Sohn’s device, mechano-node pore sensing (NPS), in a nutshell.
On the surface, her device — which looks to be about the size of a quarter — is a marvel of simplicity, using technologies from the 1960s and 1970s. Yet the data collected by mechano-NPS is expanding our understanding of cell biology in remarkable ways.
Sohn’s device enables researchers to measure the biophysical properties of cells, from their diameter to how easily they can be squished, as they flow through a maze of channels, each about one-tenth as wide as a human hair and through which current flows. As cells pass through, changes to their shape and other properties are measured by fluctuations in the current.
“Just seeing that drop off in current as a cell passes through different sections of our device, we can translate that into the size of the cell, how stiff or soft it is and how well it recovers,” says Sohn.
Sohn and her research team have shown that these mechanical properties can provide important clues about a cell’s future. A cell’s stiffness or transit time through a channel, for example, may shed light on whether that cell will remain healthy or become cancerous. For certain cancers, it could also indicate whether therapies that use a particular drug could be effective. Now, less than five years since its initial development, this simple device is already showing promise as a tool for better cancer detection and treatments.
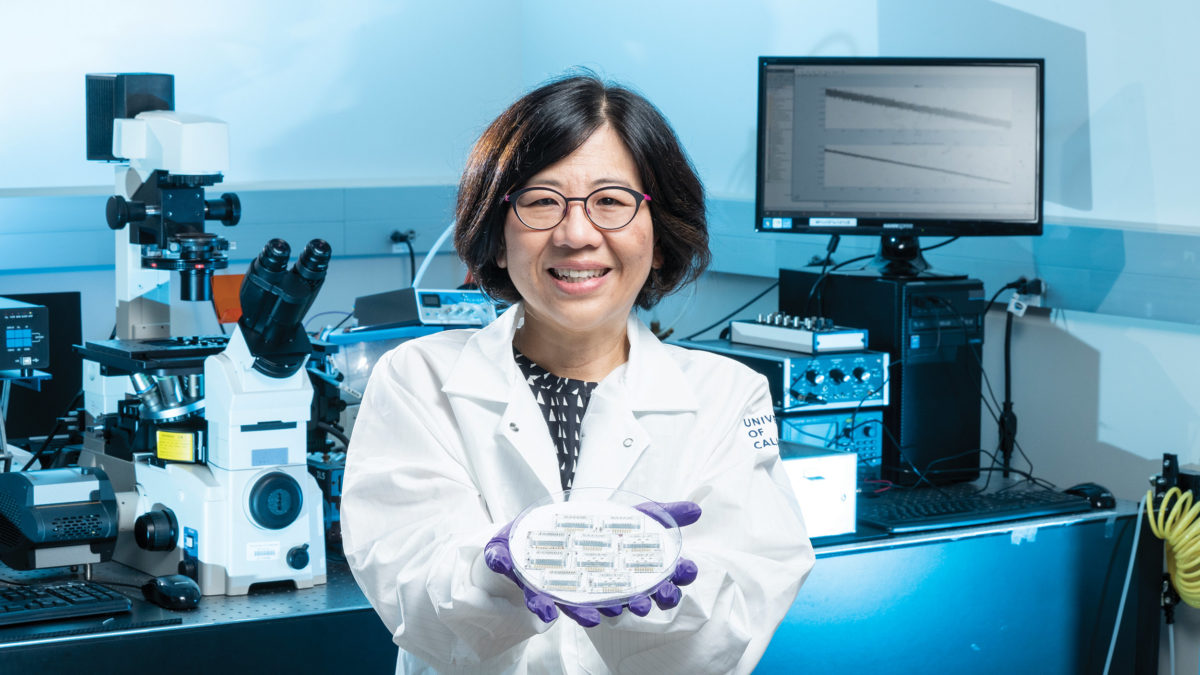
Mechanical engineering professor Lydia Sohn holds a petri dish containing mechano-node pore sensing (NPS) devices. (Photo by Adam Lau/Berkeley Engineering)
A new approach to microfluidics
Decades before Sohn developed mechano-NPS, researchers had been using microfluidic channels to measure cells and molecules. These channels, measured in microns, typically contain as little as tens of nanoliters of fluid.
Sohn and her students introduced a new approach to microfluidics in 2013. “One group of students said, ‘If this channel is like a wire, we can change its shape, and we could possibly measure different things,’” says Sohn. “And that’s how node pore sensing came about.”
The pore, or channel, used in node pore sensing has the unique ability to detect particles from tens of nanometers to several microns in size. Nodes inserted along the channel produce a series of electronic pulses as single cells pass through the device. This series of pulses is like a signature for each cell, which ensures that even the smallest particles do not pass through the device undetected, a challenge with previous microfluidic platforms.
However, if two or more cells enter a channel, signature overlaps occur, making it difficult to track data measurements to the correct cell. To assist with signal processing for the device, Sohn collaborated with Michael Lustig, professor of electrical engineering and computer sciences. “I work on MRI, but I saw that some classical ideas in signal processing of radar and digital communications could be used for this application,” says Lustig.
Together, Sohn and Lustig coded the signal for different channels, so that cells would issue special patterns as they passed through them. Researchers could then determine which cell or channel the signal corresponded to, like a cellphone tower differentiating between different signals from countless phones that are transmitting on the same frequency.
The addition of signal processing to Sohn’s device was a game changer. It resulted in significantly higher throughput — multiple cells could be pushed through the channel and studied, and multiple channels could be used, rather than a single cell at a time in a single channel. It also improved the signal-to-noise ratio, so signals from even the smallest particles could be detected.
In 2018, Junghyun Kim (Ph.D.’18 ME), then a graduate student in Sohn’s lab, developed what became the initial platform for mechano-NPS. “He wanted to measure mechanical properties of cells, and he was going to make this [new] device by modifying our general device,” says Sohn. “I said, ‘Well, okay, let’s see what happens in a couple months.’ And you know what? His instincts were right. He really opened up this whole new field for us.”
Kim demonstrated how the mechano-NPS platform could be used to simultaneously measure a single cell’s diameter, resistance to compressive deformation, transverse deformation and recovery from deformation. Using these mechanical properties, researchers could accurately differentiate between cell types and forgo the time-consuming process of attaching tags, or labels, to individual cells to identify them. In this way, mechano-NPS also proved to be a more efficient and faster way to study populations of cells.
Understanding breast cancer risk
Sohn was determined to find real-world applications for her device. “As an engineer, it’s not just about making platforms and getting data; it has to have a real use,” she says.
Colleagues suggested using mechano-NPS to study cancer cells. The relevance appealed to her, and a family history of cancer — both of her parents have been treated for the disease — factored into her decision. “If there’s an easier way to do detection and monitoring than we have now, that would help the patient and the doctor,” says Sohn.
Mechano-NPS sparked a yearslong collaboration between Sohn and Mark LaBarge, a professor of population sciences at City of Hope, a national cancer center located about 20 miles northeast of Los Angeles in the city of Duarte. LaBarge was previously a scientist at Berkeley Lab, where he met Sohn 10 years ago. Intrigued by each other’s work, they decided to use mechano-NPS to determine which women might be more susceptible to breast cancer as they get older.
LaBarge proposed using mechano-NPS on primary breast cells for women of different ages to see if they could spot a difference in the way the cells responded as they passed through the microfluidic channels. The results were startling.
“We found that in younger women, the breast cells, most of the time, recover [from being squished] much faster than older women’s breast cells,” says Sohn. “We could see the older cells just taking longer to recover.”
They then explored how the mechanical properties of the breast cells changed if they pushed them through a malignant progression — the molecular stages that a cell undergoes as it transforms from a normal cell into a cancer cell.
“Each one of those stages has its own unique mechanical portrait,” says LaBarge. “We even found that we could tell the difference between cells from a woman in her 30s versus cells from a woman in her 50s with a pretty high level of accuracy.”
After this discovery, they worked with Kim to look at breast cells obtained from a biopsy or a fine-needle aspiration to see whether cellular mechanical properties — such as deformation from passing through the microfluidic channel, or the recovery time needed to return to the original shape — indicated malignancy of cancer cells and their metastatic potential.
Their findings showed that mechano-NPS could indeed distinguish between malignant and non-malignant human breast cells. They could even measure the changes to the protein structures, or the cytoskeleton, inside the malignant cells. Also, using only these mechanical properties, Sohn, LaBarge and Kim could differentiate between cell sub-lineages and chronological age groups of normal breast cells.
“We have this theory that a woman has a chronological age, and her breast tissue has a mechanical age; how far apart those two are is going to define the true susceptibility of breast cancer,” says Sohn. “Of course, we have to prove it. But a lot of preliminary data is showing that we’re on the right track.”
“You need a lot of data to take advantage of machine learning, and that’s one thing that I think the mechano-NPS device does that no other device in mechanobiology can do — measure lots of cells very efficiently.”
With each year, they seem to be getting closer to meeting that goal. Using mechano-NPS, one of LaBarge’s postdoctoral fellows, Stefan Hinz, discovered a cytoskeletal component, a type of keratin, that is directly related to why women are more susceptible to breast cancer as they age. “We think [it] is responsible not just for the difference between young cells and old cells, but also the difference between cells in women that are likely to get cancer and those that are not likely to get cancer,” says LaBarge.
Sohn’s device can measure hundreds of cells in minutes, allowing LaBarge to study populations of cells and create algorithms for classifying them based on age. “You need a lot of data to take advantage of machine learning, and that’s one thing that I think the mechano-NPS device does that no other device in mechanobiology can do — measure lots of cells very efficiently.”
This was particularly valuable when LaBarge looked at breast cells from young women with different breast cancer-related mutations. While molecularly distinct from one another, from a mechanical point of view, they all appeared to have accelerated aging. “When we ask the machine learning algorithm to tell us if [the breast cells] are young or old, they all come out looking 20 or 30 years older than they really are,” says LaBarge.
With this newest research, LaBarge and Sohn think mechano-NPS could make the leap from the lab to the clinical setting. “We might be one or two grant cycles away from translating the device from being a benchtop wunderkind into being something more like a clinical trial to assess cancer risk,” says LaBarge.
“What is it telling us?”
Mechano-NPS has also proved useful in research related to the diagnosis and treatment of acute promyelocytic leukemia (APL), an aggressive blood cancer. Once a person with APL presents with the acute phase, they need to be given a drug called ATRA (all-trans retinoic acid), or they will likely die within a week. But there is a small set of APL patients who receive ATRA but don’t respond or stop responding to it, and there are no biological assays to test for ATRA resistance.
“That’s where our device came through,” says Sohn. “Brian Li, a [former] graduate student [in my lab], wanted to know if we could detect ATRA resistance in APL cells using mechanical measurements.”
They discovered that ATRA-resistant APL cells are significantly stiffer than ATRA-sensitive APL cells. They also studied the biological reason why cells are soft or stiff and how the internal components, such as the nucleus and cytoskeleton, correspond to whether an APL cell is resistant to ATRA.
For Sohn, the intersection between physical and biological properties is not only fascinating, but also holds a lot of promise. “This mechanical property of cells is making a niche for itself in applications,” says Sohn. “It’s opened our thoughts on what it means for a cell to be soft or stiff. What’s exactly going on inside this cell? What is it telling us?”
These days, you can find Sohn working on new applications for her mechano-NPS device in a range of fields. She recently collaborated with associate professor of mechanical engineering Grace O’Connell, whose research is focused on soft tissue biomechanics and tissue regeneration.
“We set up a platform in her lab, so that they could look at the mechanical properties of her chondrocytes [cells found in cartilage], and whether or not they can use stiffness as a parameter to select the appropriate chondrocytes for potential tissue regeneration,” says Sohn.
Sohn also has been working with Andreas Stahl, professor in the Department of Nutritional Science and Toxicology. His team is studying how drugs applied to adipocytes — fat cells that make up adipose tissue — can change the stiffness of the cells. They would typically use an atomic force microscope for their work, but Sohn’s device is allowing them to increase their productivity.
“Every time I think we’ve done enough with this device, there’s always something new that comes on board,” says Sohn. “It’s very satisfying to just keep going and see what happens. It’s so simple — and that, I think, is really cool.”