Rubinsky goes global with health care reform

A Berkeley professor for three decades, Boris Rubinsky in 2006 established the Center for Bioengineering in the Service of Humanity and Society at Hebrew University of Jerusalem, which unites students from diverse backgrounds to do bioengineering research focused on underserved populations. (Photo by Bart Nagel.)
Inventor, researcher and educator Boris Rubinsky has taken his show on the road.
During three prolific decades in Berkeley’s labs and classrooms, the professor of bioengineering and mechanical engineering stacked up nearly 40 patents and cofounded half a dozen startups in surgical techniques, bionic technology and imaging. He has advised more than 70 graduate students, many of whom today hold leadership positions in academia and industry.
Now Rubinsky is finding inspiration in his new role as health care advocate for the economically disadvantaged, a self-described modern-day Johnny Appleseed pitching his elegant devices and procedures designed to simplify complex medical imaging and treatment techniques. He is training fellow researchers, surgeons, students and health ministers, building endorsement for his conviction that inexpensive but scientifically advanced technologies can improve health care for underserved populations from tiny Indian villages to deep in Chicago’s inner city.
“Sixty percent of people who need cancer treatment don’t have access to sophisticated treatments,” Rubinsky says. “By the time these huge tumors are detected, it is too late. Even palliative techniques do not exist.”
According to the World Health Organization (WHO), industrialized countries have an increasing incidence of cancer and twice the cancer diagnoses as developing nations due to behaviors like smoking and fatty diets and exposure to carcinogens. But in the developing world—due to lack of education, poor hygiene, rudimentary health care and limited resources—80 percent of cancers are late-stage, incurable tumors by the time they are detected. Such cancers can also occur in America’s urban poor.
“Technology and society don’t pay attention to the needs of the economically disadvantaged,” Rubinsky says. “I spread the word that advanced technologies should be developed with these people in mind.” The Romanian native says he was powerfully driven by his experience as the child of Holocaust survivors.

Rubinsky explains the technique of irreversible electroporation, a minimally invasive surgical procedure he developed in 2002 that uses microsecond-long electrical pulses to destroy cancerous tumors without harming adjacent organs, vessels or nerves. (Photo by Bart Nagel.)
“My mother was in a concentration camp from the age of 18, and somehow, my entire life was centered around her suffering,” he recalls. “I saw bioengineering as one way you could directly produce benefits for human beings, and I was right. When you build a better car, it is valuable, it is good. But when you build a machine that saves a life, that’s a different thing.”
To support his vision, in 2006 Rubinsky established the Center for Bioengineering in the Service of Humanity and Society at Hebrew University of Jerusalem, where he brings students together from diverse backgrounds, including Arabs and Jews, to collaborate on bioengineering projects. His work has garnered considerable international attention; he has visited India, Mexico, and small villages in Eastern Europe and the Palestinian territories and has received invitations to collaborate with hospital networks and health ministries in Vietnam, Rwanda and other African countries, and South and Central America. Wherever he goes, he says, his UC Berkeley credentials give him the respectability and visibility he needs to accomplish his goals.
“I didn’t get this sense when I used to spend day and night in my lab in Etcheverry Hall and never go out,” Rubinsky says. “But since I began traveling the world, I realized what a powerhouse Berkeley is and what a great reputation it has. Now I am more proud than ever to be affiliated with Berkeley.”

Surgeon Gary Onik performs irreversible electroporation, the procedure developed by Rubinsky that has now been used to treat 104 patients with cancers of the liver, kidney, lung, brain and pancreas, many of which would have been inoperable with mainstream surgeries. (Photo by Boris Rubinsky.)
The Silverman decade
Rubinsky refers to his most recent work at Berkeley as the Silverman decade, after Arnold and Barbara Silverman, two UC Berkeley alumni who in 2000 endowed a distinguished professorship in bioengineering that Rubinsky has held for the last 10 years (see below). His early work had focused on bioelectronics and cryosurgery, but all that changed in 2002, when he discovered non-thermal irreversible electroporation (IRE). He got so excited about its potential to revolutionize cancer treatment that he dropped his cryosurgery research.
“The technology is extremely simple for both physician and patient,” Rubinsky explains. “It is almost miraculous; when surgeons see it for the first time, they cannot believe it.”
Electroporation involves inserting into a tumor two slender electrodes connected to an electrical generator, then producing quick electrical pulses of an amplitude and wavelength that create nanoscale holes, or pores, in the tumor’s cell membranes. The minimally invasive procedure can be guided by a new imaging technique, electrical impedance tomography, also invented by Rubinsky. And for reasons that must be further explored, he says, IRE appears to mobilize the immune system to recognize and naturally remove the dead cells after about two weeks.
The problem with mainstream cancer treatments like cryotherapy, which he had been working to refine, is that they cause collateral damage. In prostate cancer, for example, the urethra and nearby nerves might be damaged, leading to incontinence and sexual impotence. Pancreatic tumors are situated near the colon and major blood vessels. But IRE exclusively targets the tumor’s cell membranes, leaving critical organs, vasculature, ducts and nerves completely unharmed.
“This treatment is valuable for any place in the world, but particularly for economically disadvantaged areas because it is quicker and cheaper,” Rubinsky says. “You don’t need advanced technology and clinical skills. A nurse who knows how to use a syringe could do it.”
While electroporation was not new, it was being used primarily to open cell membranes temporarily to introduce gene or drug therapies. Rubinsky discovered that longer and stronger pulses could produce pores that didn’t close back up, causing the cancerous cells to lose their homeostatis and die.
Because it targets specific molecules, Rubinsky calls IRE the first “molecular” surgery in the world. Approved by the FDA in 2006 and now in testing at 25 research universities (including UCLA), it has been used successfully to treat 104 patients for cancers of the prostate, liver, kidney, lung, brain and pancreas, many of which would have been inoperable without it. Some patients treated for prostate cancer got up and drove away 30 minutes later, with no incision or pain, no incontinence or impotence—only a bruise at the tumor site, Rubinsky says.
He commercialized the technology (for which UC Berkeley holds all the patents) with collaborator Gary Onik, at the time director of surgical imaging at Florida Hospital Celebration Health. Their company, Oncobionic, sold in 2008 to New York–based AngioDynamics. Rubinsky just published a major medical text on the technique and, based on experience with his prior inventions (like imaging-monitored cryosurgery, with which Desmond Tutu was treated in 1999), he believes IRE could be widely practiced in about three years. It also holds promise for ablating other solid masses, he says, like arterial plaques and ocular melanomas.
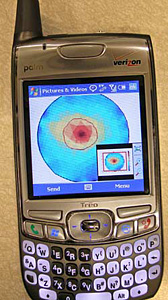
To drive down the cost of medical testing in remote areas, many of Rubinsky’s recent inventions use cellular phones to transmit images and data like this simulated breast tumor, shown in red. For a video of Rubinsky describing the technology, go here. (Photo by Boris Rubinsky.)
Can you heal me now?
Curing cancer is big news. But Rubinsky’s April 2008 paper in the online journal PLoS One about his new cell phone–based medical imaging system went positively viral.
The engineer in him is always driven by the data; in this case it was WHO statistics reporting that up to three-quarters of the world population lacks access to medical imaging, which is critical for curative therapy in 20 percent of disease. Although some clinics in the developing world have received donations of medical imaging equipment, half of it doesn’t work within a year due to poor maintenance and lack of spare parts. But everyone has a cell phone.
“I had just visited Mexico,” Rubinsky says, “and my host told me that the first thing people there spend their salary on is their cellular phone bills. You can be anywhere, even in the foothills of the Himalayas, and everywhere you see cellular phones.” Piggy-backing onto that existing infrastructure means the imaging system would cost hundreds of dollars rather than tens of thousands and could be used by any nurse in any small rural clinic.
Medical imaging devices generally have three components: the data acquisition hardware, or transducer, which is placed on the patient’s body to gather data; the image processing software, the most sophisticated component; and a monitor to display data and images. Rubinsky’s team decoupled these parts to drive down cost. Using the cell phone as a monitor and a remotely accessed medical center to process the data, all they needed was the transducer; they used a commercially available standard transducer that cost a fraction of an entire ultrasound device.
“If a physician comes to a small village, all he needs in his pocket is this transducer, which is about seven inches long and one inch in diameter, to pass over the body part to be checked,” Rubinsky explains. “Then the data are sent through the cell phone to a central facility and processed into an image that is transmitted back to the physician or a radiologist.”
His latest invention (for which the UC Berkeley–owned patent was just issued last December 29) was similarly inspired by WHO data, this time on the one in four women worldwide who die post-partum due to undetected internal bleeding. The device consists of two coils worn by the subject that noninvasively detect fundamental physical changes and frequency-dependent electrical currents in abnormal tissue. The raw data are sent through the cell phone to any major hospital or treatment center in the world. The device has been similarly used to detect bleeding in the brain.
Other projects in the works include a wristwatch-like cognitive analysis device that quietly monitors the body for measurements like blood-sugar levels in diabetics or alertness in drivers or pilots. (It received first prize in the 2008 CITRIS Big Ideas competition.) How about a cell phone–based medical imaging system for at-home detection of breast and prostate cancer? Rubinsky keeps the new concepts coming, any of which could have multiple applications from Indian villages to rural Indiana.
Although he retired early from his College of Engineering position to realize his dream of establishing the Center for Bioengineering in the Service of Humanity and Society, he maintains strong ties to Berkeley, where he is Professor of the Graduate School. He is now working to establish at Berkeley an international alliance with other universities to unite students in performing the work of the new center. Hebrew University and Al-Quds University (the Arab University in Jerusalem), for example, would be more likely to work together if there were a neutral academic center leading the charge.
“When new places hear about [the center], they want in,” Rubinsky says. “Young people absolutely feel the need to participate in such activities. Palestinian and Israeli students are working together, and there is real excitement on both sides. We are doing something worthwhile for both the world and for their mutual understanding. It’s an extraordinarily satisfying feeling.”
How to sustain our engineering faculty
Arnold Silverman (B.S.’60, M.S.’61 EECS) and Barbara Silverman (B.A.’60 Socio., Edu. Cred.’61) of Atherton, California, are Berkeley alumni and strong supporters of the campus and the College of Engineering. They are helping to sustain the college by endowing faculty chairs and supporting the superior research of the engineering faculty.
In 2000, the Silvermans had the vision to establish a distinguished professorship in bioengineering to support the continuing competitiveness of U.S. technology worldwide and progress in health care reform. In 2008, they also created a new chair, the Arnold and Barbara Silverman Chairmanship in Bioengineering, held by Matthew Tirrell, who last July was appointed chair of the department.
“Arnold and Barbara Silverman have given generously to enable the kind of visionary work done by Boris Rubinsky,” Tirrell says. “Support that allows faculty and students to explore their most creative ideas, without the overhead of government grants and contracts, is the most precious kind of support in a university.”
Berkeley established its Department of Bioengineering in 1998; since then, the department has grown from only two core faculty to 19, from one class to more than 30, and from 387 student applicants to more than 1,200. The U.S. Department of Labor predicts that between 2006 and 2016, the number of bioengineering jobs will increase by 21 percent.
If you are interested in more information on how to establish an endowed faculty chair, please contact Engineering College Relations at 510-642-2487.